How Psychedelics Are Revolutionizing Treatment for PTSD, Anxiety, and Depression. In recent years, psychedelic substances like psilocybin (found in “magic mushrooms”) and MDMA (commonly known as ecstasy) have emerged as powerful potential therapies for some of the most stubborn mental health challenges: post-traumatic stress disorder (PTSD), anxiety, and treatment-resistant depression. Unlike traditional antidepressants that often take weeks to work and fail for many patients, these compounds show rapid, profound, and lasting effects by rewiring the brain at a fundamental level.




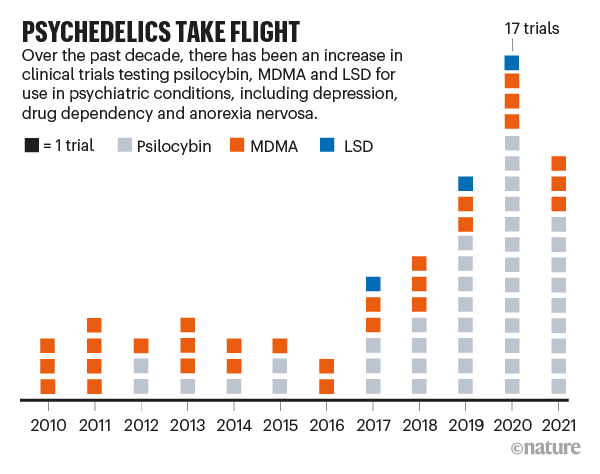
Clinical trials have demonstrated remarkable promise. MDMA-assisted therapy has been particularly effective for PTSD, helping patients process traumatic memories without overwhelming fear. Psilocybin has shown strong results in alleviating anxiety and depression, even in terminal illness patients, by fostering a sense of connectedness and reducing existential dread. These treatments often involve guided sessions in a therapeutic setting, where the psychedelic experience facilitates deep emotional breakthroughs.


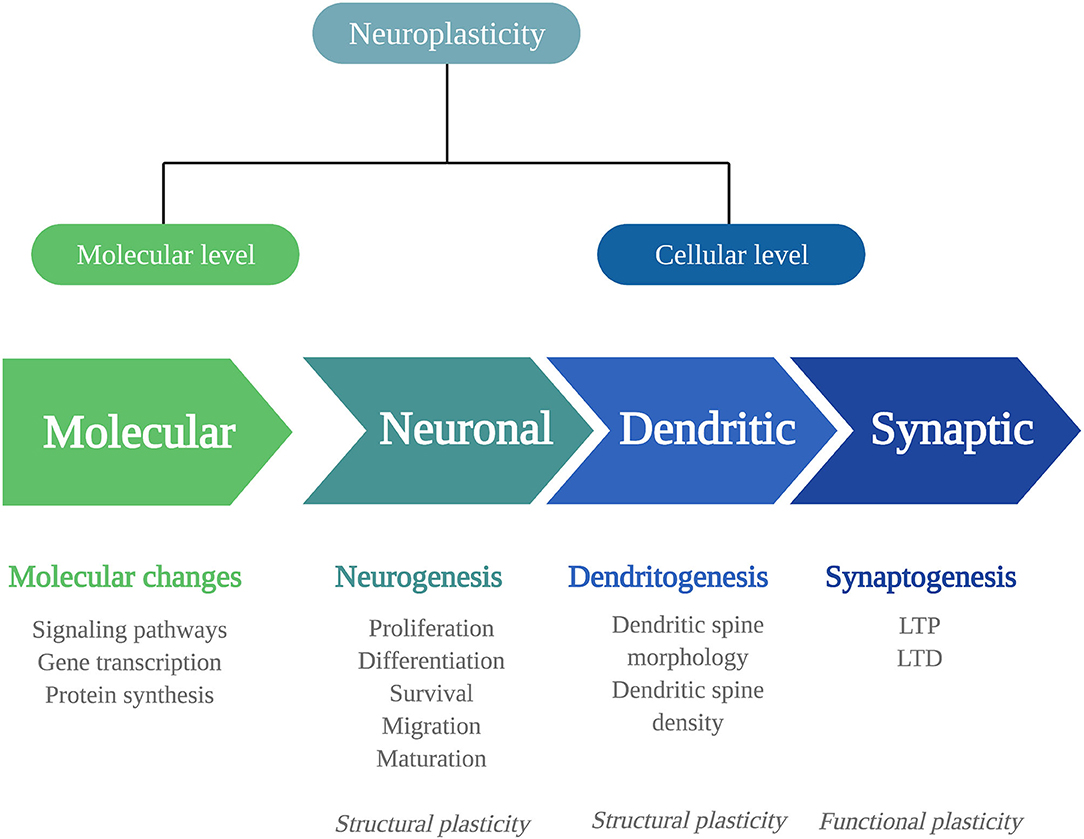
But how do these substances achieve such transformative effects? The key lies in their ability to promote neuroplasticity—the brain’s capacity to form new connections between neurons, essentially “rewiring” rigid patterns associated with mental illness.
The Science of Brain Rewiring: Internal Receptor Activation
At the heart of this mechanism is the 5-hydroxytryptamine 2A receptor (5-HT2AR), a protein found both on the surface and inside brain cells. Groundbreaking research from Dr. David Olson’s team at the University of California, Davis, published in Science (February 17, 2023), reveals why psychedelics uniquely drive plasticity.
Receptor Location Matters for Psychedelic Drug Effects | UC Davis
Unlike serotonin (the neurotransmitter targeted by many antidepressants), which binds only to surface receptors and has limited plastic effects, psychedelics like psilocybin and certain non-hallucinogenic analogs can cross the neuron’s membrane to activate internal 5-HT2ARs.
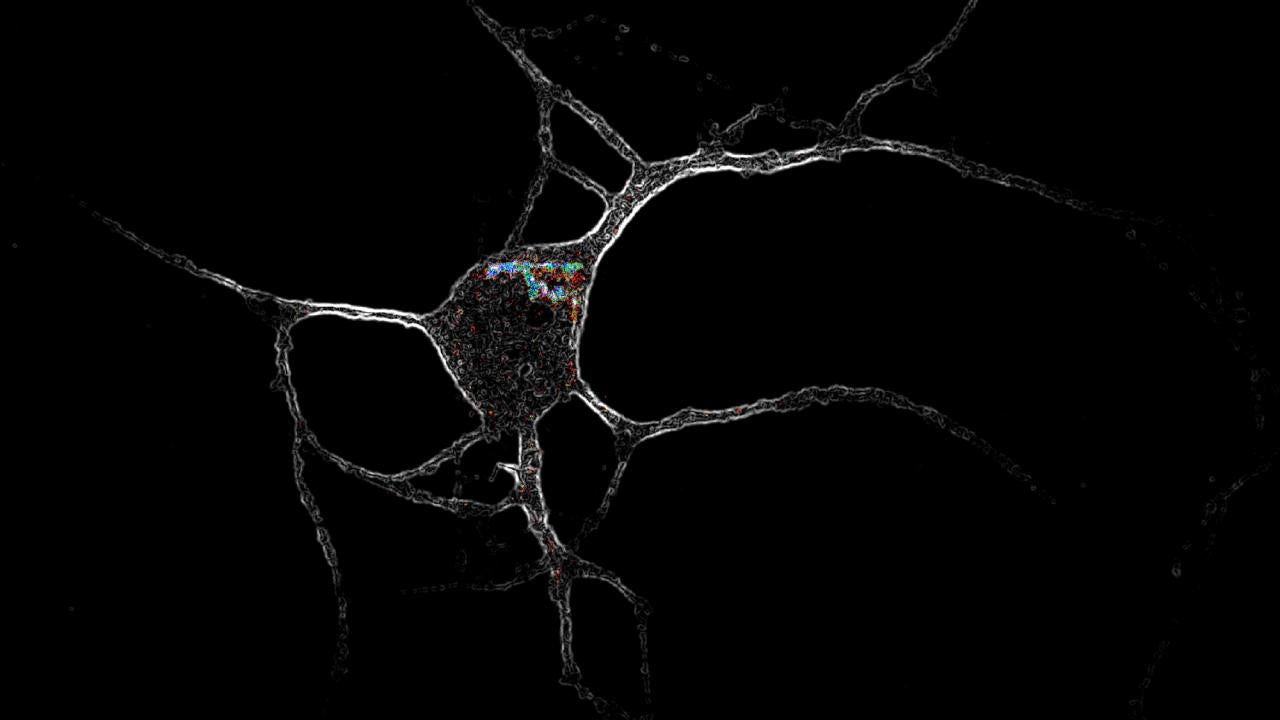
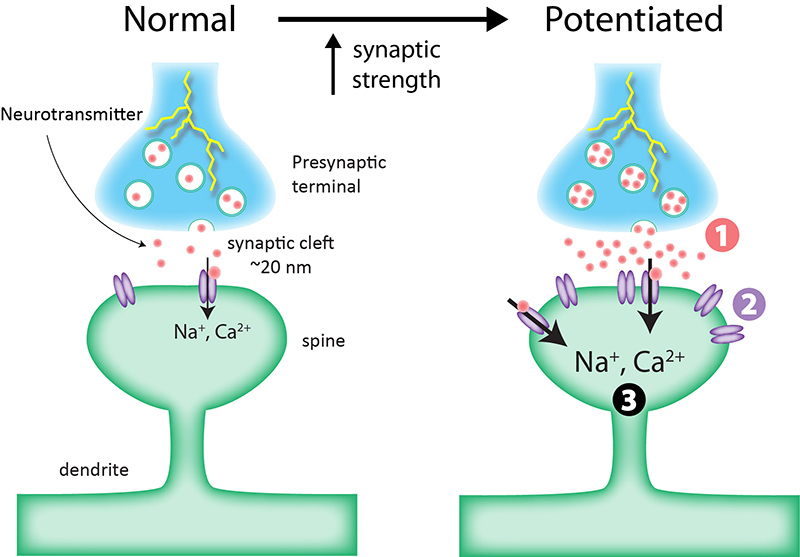
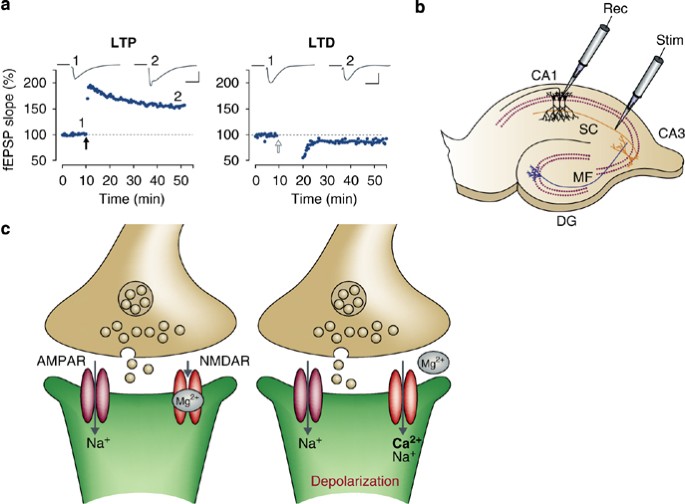
This internal binding triggers distinct signaling pathways that promote the growth of dendritic spines—tiny protrusions on neurons that form synapses, the connections enabling communication across the brain.
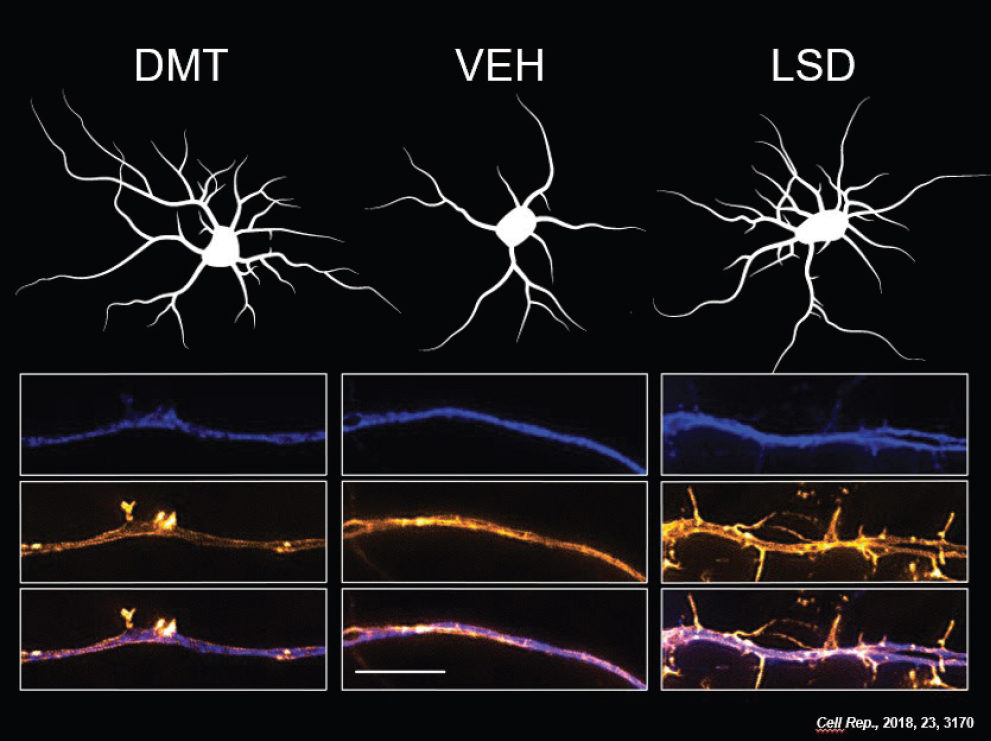

Experiments showed that compounds penetrating the cell membrane dramatically boosted dendritic spine formation, while those restricted to the surface (like serotonin) did not. When researchers artificially allowed serotonin inside cells—via electrical currents or engineered proteins—it suddenly gained plasticity-promoting powers.
In living mouse models, enhancing internal serotonin access led to increased dendritic spines in key brain regions and behavioral improvements linked to reduced depression-like symptoms.
A Path to Safer, Hallucination-Free Therapies
This discovery explains why some 5-HT2AR-binding drugs cause hallucinations (via surface activation) while others promote healing plasticity (via internal activation). It opens the door to designing “next-generation” psychoplastogens—drugs that harness brain-rewiring benefits without intense psychedelic experiences.
As Dr. Olson notes, “These results give us deeper mechanistic insight into how the receptor promotes plasticity, and may allow us to design better drugs.”
While more research is needed to ensure safety and separate therapeutic from hallucinogenic effects, this work illuminates a profound truth: psychedelics don’t just mask symptoms—they help the brain heal itself by restoring its innate flexibility. For millions suffering from PTSD, anxiety, and depression, this could mean not just relief, but true renewal.